Abstract
Background: Relapsed or refractory AML is associated with a dismal prognosis and refinement of re-induction strategies is needed. Data on outcomes stratified by molecular cohort in the relapsed or refractory setting are scarce. The aim of this study is to contribute evidence toward the optimal re-induction strategy in the relapsed/refractory setting and to characterize outcomes on the basis of molecular cohorts.
Patients & Methods: We analyzed 59 patients that underwent treatment for relapsed or refractory (R/R) AML from January 2016 to December 2021 at VCU Massey Cancer Center. Patients were divided into two cohorts: patients that received FLAG-IDA vs those that received MEC. Within both categories, patients were sub-stratified by molecular aberration as numbers allowed. Baseline demographics were obtained, including age, performance status, and comorbidities as well as disease characteristics, including molecular profiling, alongside cytogenetic risk, doses of induction regimens, response, and survival. Patients were considered evaluable for response if there was a bone marrow biopsy following a minimum of 28 days of treatment. The event for calculating the overall survival (OS) was the date of death and patients were otherwise censored at last date of contact.
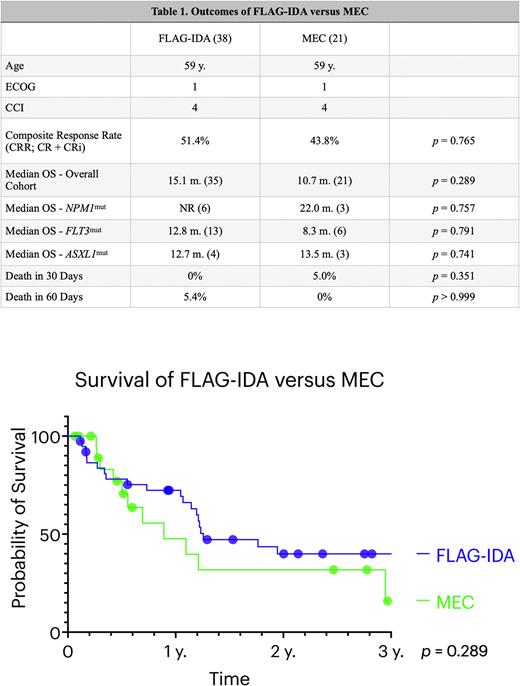
Results: There were 38 patients treated with FLAG-IDA in the R/R setting. Twenty-eight (78.9%) were treated for refractory disease and 21.1% were for relapsed disease. The median age was 59 years, median ECOG score was 1, and median Charlson Comorbidity Index (CCI) score was 4. The composite response rate (CRR; CR+CRi) was 51.4% at the time of the end-of-treatment marrow. The median OS for the FLAG-IDA cohort was 15.1 months. We then stratified survival by molecular cohort and identified that NPM1mut had an OS that was not reached (NR) at a median follow-up time of 18.4 m, FLT3mut (including ITD, TKD, and NOS) had an OS of 12.8 m., and ASXL1mut had an OS of 12.7 m. There was no difference between NPM1mut and FLT3mut cohorts with respect to survival. There were no deaths in 30 days and 5.4% died within 60 days. There were 21 patients treated with MEC for relapsed/refractory disease. Thirteen (61.9%) were treated for refractory disease and 38.1% were treated for relapsed disease. The median age was 59 years, median ECOG score 1, and median CCI score 4. The CRR was 43.8% and the median OS was 10.7 m. When molecularly stratified, the OS of NPM1mut was 22.0 m., FLT3mut 8.3 m., and ASXL1mut 13.5 m. A total of 5.0% of patients died within 30 days and there were no deaths within 60 days. While FLAG-IDA appeared to improve the OS by 4.4 months compared to MEC, there was no significant difference in OS between FLAG-IDA and MEC reinduction (p = 0.289).
Conclusions: There is currently little data to guide treatment choices among several intensive regimens in the R/R AML setting, and this decision is largely driven by physician or institutional preference. In the setting of the ongoing fludarabine shortage, non-fludarabine based regimens are needed to be able to quickly and effectively treat these patients. Our study demonstrates no statistically significant difference in CRR or OS between FLAG-IDA or MEC at our institution, with similar findings across a variety of molecular cohorts. However, this data must be interpreted with caution given the retrospective nature and sample size.
Disclosures
Maher:BMS: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal